This press release was written by Leigh Cooper in University of Idaho Communications and Marketing. View the original press release here. See the article published in the Idaho Press here. Dr. Marty Ytreberg is the Associate Director of IMCI.
MOSCOW, Idaho — April 20, 2020 —The University of Idaho is working to identify a cure for coronaviruses, including COVID-19.
The Department of Biological Sciences team expects to finish preliminary tests within a year. Researchers will also develop a pipeline for identifying drugs that block viruses from infecting human cells.
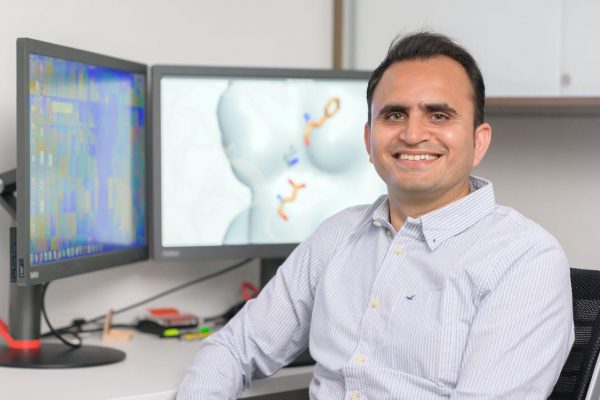
The project is funded with $100,000 from a National Science Foundation EPSCoR grant issued to U of I Department of Physics Professor Marty Ytreberg. The EPSCoR funds were provided to determine how amino acid changes modify the way proteins interact with other molecules.
“Funding agencies are giving leeway to researchers with existing grants to shuttle resources toward the COVID pandemic,” Ytreberg said. “We decided this was a good investment, because it has the potential to lead to a therapeutic and fits within the theme of the grant.”
The team includes molecular modeling specialist Jagdish Patel, a research assistant professor; virologist Paul Rowley, an assistant professor; and evolutionary biologist JT Van Leuven, a research assistant professor. The research is being conducted within the Institute for Modeling Collaboration and Innovation, U of I’s multidisciplinary, collaborative research program that houses biomedical research modeling experts.
“The University of Idaho’s research engine has pivoted quickly in the battle against COVID-19,” President Scott Green said. “I’m proud of this team for taking the initiative to help develop a cure for this virus. Their work is rising to the challenge we all face during this difficult time and will help save countless lives in the process.”
The team hopes to create a drug that shields human cells rather than attacks viruses. The severe acute respiratory syndrome coronavirus (SARS-CoV-2) virus is shaped like a ball with spikes on the surface as shown in widely-used photos. The spike proteins have evolved to dock with a specific protein — called the ACE2 receptor — on the surface of human cells. The attachment of the spike protein to ACE2 begins the infection process by which the virus transfers genetic material to the cell. This genetic material tricks the cell into generating more virus.
Patel and his team want their drug to shield the ACE2 receptor from interacting with the SARS-CoV-2 spike protein.
Drugs targeting human cells, as opposed to viruses, are likely to be effective for a longer period of time, Patel said. Viruses can rapidly evolve at their binding sites to render antiviral drugs ineffective.
The team will improve the known molecules and screen a large library of molecules on computers that might act as inhibitors for SARS-CoV-2. They will test potential inhibitor molecules against a SARS-CoV-2 pseudovirus, a harmless virus with SARS-CoV-2 spike proteins. Promising molecules would then be sent out for testing against the real SARS-CoV-2 virus and subsequently for clinical studies.
“The ACE2 receptor is being used by other coronaviruses as well,” Patel said. “If we find a drug that blocks SARS-CoV-2, the drug should have multiple purposes, protecting us from other coronaviruses like those that cause mild to severe respiratory infection, SARS and NL-63.”
Through the process of studying and testing potential inhibitors to combat COVID-19, the team will have developed and refined a multidisciplinary pipeline for antiviral drug development during future outbreaks.
“With the pipeline in place, we will also be able to respond much more quickly to any other disease outbreaks,” Patel said. “We’re designing the pipeline to be flexible so we can adjust to the different challenges each virus poses.”
Within their new pipeline, the researchers will identify antiviral drugs for human receptors other than ACE2, inhibitors that target the virus instead of human cell receptors and inhibitors for other animal viruses.
The awards are made through NSF EPSCoR as part of its Research Infrastructure Improvement (RII) Track-2 investment strategy. RII Track-2 is intended to build national research strength by initiating research collaborations across institutions in two or more EPSCoR jurisdictions. EPSCoR is a program designed to fulfill NSF’s mandate to promote scientific progress nationwide.
This project, “Using biophysical protein models to map genetic variation to phenotypes,” was funded under National Science Foundation grant No. OIA-1736253. The total amount of federal funds for the project is $6 million, which amounts to 100 percent of the total cost of the project.